A brain tumour is a mass of abnormal cells in the brain. Skull, which encloses the brain, is very rigid. Any growth inside such a restricted space can cause problems.
Brain tumours (BT) can be divided into primary and secondary tumours. Primary BT refers to a tumour that originates from the brain tissue and remain inside the brain. This is further divided into non-cancerous (benign) and cancerous (malignant) tumours.
Secondary brain tumours, also known as a metastatic brain tumour, occurs when cancer cells spread to brain from another organ. Metastatic tumours are considered cancer and are malignant. Secondary brain tumours most often occur in people who have a history of cancer. Rarely, a metastatic brain tumour may be the first sign of cancer that began elsewhere in your body. In adults, secondary brain tumours are far more common than are primary brain tumours.
Any cancer can spread to the brain, but common types include:
• Breast cancer
• Colon cancer
• Kidney cancer
• Lung cancer
• Melanoma
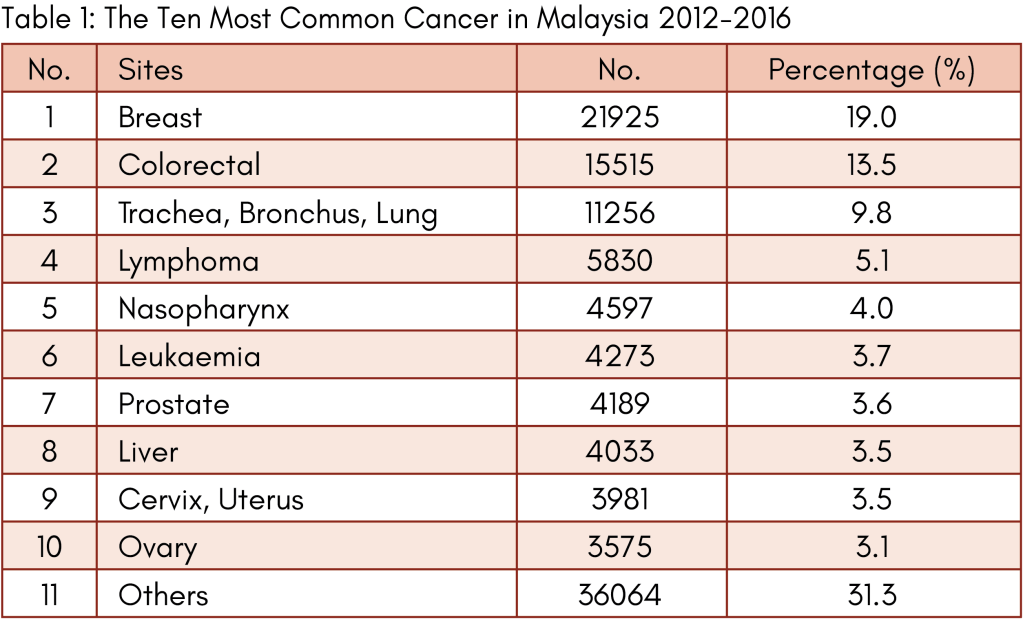
Data from the Malaysian National Cancer Registry Report (MNCRR) for 2012-2016 revealed a total number of 2,097 cases of brain BT among the Malaysians with 1,117 cases among males and 908 cases females, which ranked as 11th and 13th most common cancer among males and females respectively.
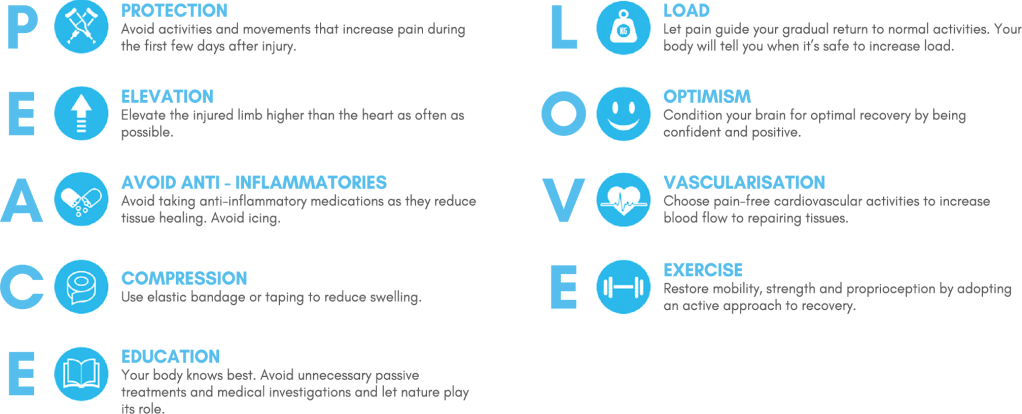
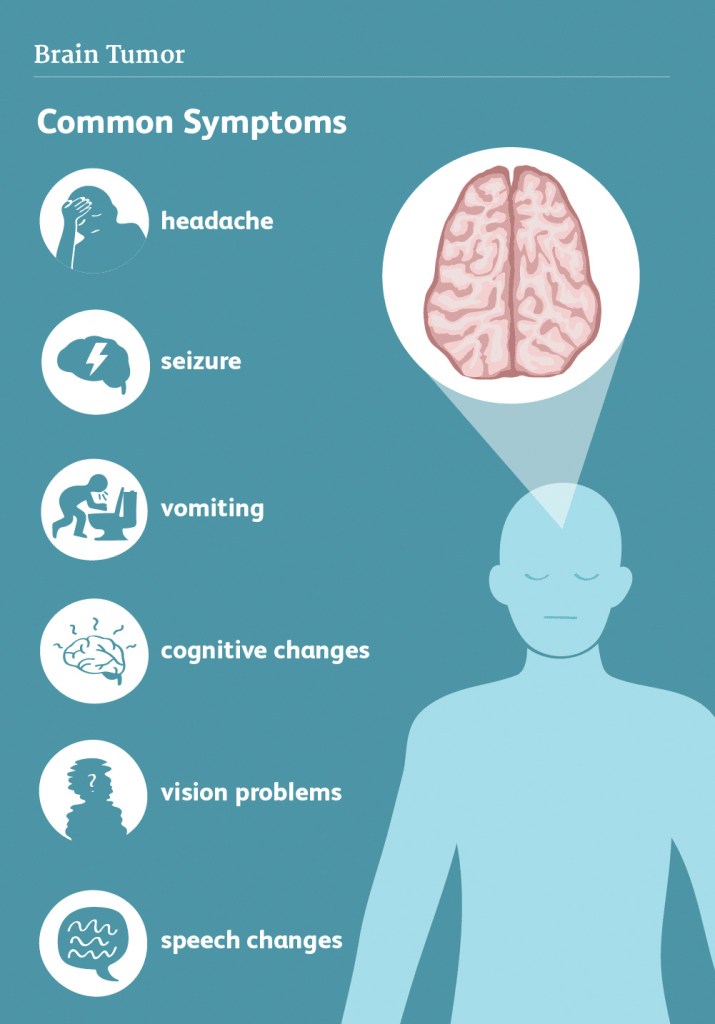
There are many symptoms of brain tumour. The early warning signs of a brain tumour can vary depending on the location of the tumour and the functional system (e.g., motor, sensory, language) it affected. Usually, the specific neurological effects of brain cancer may be associated with the brain tumour’s location or with compression of a certain area of the brain. For instance, a brain tumour near the optic nerve may result in visual problems but potential signs can include weakness, the ability to think, concentrate and balance problems. Individuals with brain tumours may also experience seizures and mental confusion.
But symptoms of brain cancer may not always match up to the tumour location—a brain tumour may cause more compression elsewhere, and the symptoms may correspond to the region of compression, not the area of the cancer.
Any considerably large brain tumour may cause several symptoms because of the pressure produced by the mass. Swelling in the brain caused by the brain tumour or surrounding inflammation may also result in specific symptoms.
Common symptoms of brain tumour may Include:
• A headache gets worse over time and certain time of the day
• Seizures
• Difficulty walking
• Numbness in part of the body
• Nausea and vomiting
• Memory loss
• Muscle weakness
• Blurring of vision, double vision or vision problems
• Difficulty in speaking
• Mood and personality changes
• Tiredness
• Gradual changes in emotional response and intellectual capacity
Some symptoms may be caused by other diseases. The only way to tell for sure is to get tested. Brain cancer may develop overtime, without any obvious signs or with mild symptoms, but it may also suddenly cause severe and fast deterioration.
Imaging tests can help to differentiate if the tumour is a primary brain tumour or secondary cancer that has spread to the brain from elsewhere in the body. Imaging tests show pictures of the inside of the body.
Few factors need to consider when choosing a diagnostic test:
• Type of tumour
• Signs and symptoms
• Age and general health
• The results of earlier medical tests
With advancement in imaging techniques can pinpoint brain tumours. Diagnostic tools include computed tomography (CT or CAT scan), Positron Emission Tomography (PET scan) and magnetic resonance imaging (MRI).
CT scan using x-ray to takes images of the inside of the body from different angles. A computer software will reconstruct these pictures into a detailed, 3-dimensional image that shows any abnormalities or tumours. A CT scan can help find blood clot inside the brain and accumulation of fluid in the fluid-filled spaces of the brain, called ventricles. Any bone changes in the skull can also be seen on a CT scan. Sometimes, a contrast medium (dye) is given into patient’s vein (intravenous) before the scan to provide better detail on the image.
Positron emission tomography (PET) or PET-CT scan is used at first to find out more about a tumour while a patient is receiving treatment. It may also be used if the tumour comes back after treatment. A PET scan is usually combined with a CT scan, called a PET-CT scan. A small amount of a radioactive substance is injected into the patient’s body. This substance is taken up by tumour cell as they are actively dividing (growing), they absorb more of the radioactive substance. However, the amount of radiation in the substance is too low to be harmful. A scanner then detects this substance to produce images of the inside of the body.
Magnetic resonance imaging (MRI). An MRI uses magnetic fields, not x-rays, to produce detailed images of the body. A special dye called a contrast medium is given into patient’s vein before the scan to create a clearer picture. MRIs create more detailed pictures than CT scans and are the preferred way to diagnose a brain tumour. The MRI may be of the brain, spinal cord, or both, depending on the type of tumour suspected and the likelihood that it will spread in the brain and spinal cord. There are different types of MRI, doctor will helps determine which type of MRI to use.
A functional MRI (fMRI) provides information about the location of specific areas of the brain that are responsible for muscle movement and speech. During the fMRI examination, the patient is asked to perform certain tasks that cause changes in the brain activity and can be seen on the fMRI image. This test is used to help plan surgery in order to avoid damaging the functional parts of the brain while removing the tumour.
Magnetic resonance spectroscopy (MRS) is a test using an MRI that provides information on the chemical composition of the brain. It can help tell the difference between any dead tissue caused by previous radiation treatments and new tumour cells in the brain.
A sample of the tumour’s tissue is the only definitive way a brain tumour can be diagnosed. A sample of tumour tissue for examination under a microscope by a pathologist, a doctor who specialises in interpreting laboratory tests and evaluating cells, tissues, and organs to diagnose disease. A biopsy can be done as part of surgery to remove the entire tumour. Or surgery may be done as a separate procedure if completely removing the tumour is not possible because of its location or a patient’s health.
Treatment for brain tumours depends on the specific size and type of the mass as well as the patient’s specific tolerance for medications. Treatment options include medications to control seizures, surgery and steroid medications, as well as radiation and chemotherapy. Individuals with tumours that have the potential to grow rapidly may benefit from targeted therapy treatments in which specific parts of the cell are treated to hinder their growth.

Dr. Ch’ng Chee How
Neurosurgeon
MB BCh BAO (NUI), M.Surg. (Neurosurgery) (USM), Clinical F’ship in Skullbase & Braintumor (Korea)
Dr. Ch’ng Chee How is a resident Consultant Neurosurgeon with special interests in Brain Tumour and Minimally Invasive Endoscopic Skull Base Surgery.
He has gained vast experience in Brain and Spine Surgery from working at various tertiary neurosurgical centres including Hospital Pulau Pinang, Hospital USM, Hospital Kuala Lumpur, Hospital Sultanah Aminah (Johor) and Hospital Queen Elizabeth (Sabah). In 2018, he was conferred the Excellent Service Award from Hospital Pulau Pinang for exemplary overall performance.