Introduction:
Diabetic retinopathy, a complication arising from diabetes, affects the eyes by causing damage to the blood vessels in the retina, the light-sensitive nerve at the back of the eye. Despite often exhibiting no symptoms in its early stages, diabetic retinopathy can lead to severe vision issues and, if left untreated, even blindness. Both type 1 and type 2 diabetes can predispose individuals to diabetic retinopathy, with the risk increasing based on the duration of diabetes and inadequate blood sugar control.
This article aims to provide an overview of diabetic retinopathy, its causes, symptoms, stages, risk factors, complications, and the importance of timely eye examinations for effective management.
Causes:
The primary cause of diabetic retinopathy is elevated blood sugar levels, leading to the gradual blockage of capillaries that supply blood to the retina. This process triggers the growth of abnormal blood vessels prone to leakage.
Symptoms:
Diabetic retinopathy may initially be asymptomatic, but as the condition progresses, the following symptoms may emerge:
– Floaters or dark lines in your vision.
– Blurred vision.
– Vision fluctuations.
– Dark or blank areas in your field of vision.
– Vision loss.
Stages:
Diabetic retinopathy has two stages:
1. Early diabetic retinopathy, also known as nonproliferative diabetic retinopathy (NPDR), where abnormal new blood vessels have not yet formed.
2. Advanced diabetic retinopathy, or proliferative diabetic retinopathy, characterised by the growth of abnormal blood vessels in the retina.
Risk Factors:
Several factors can increase the risk of diabetic retinopathy, including the duration of diabetes, poorly controlled blood sugar levels, hypertension, high cholesterol, pregnancy, and tobacco use.
Complications:
Diabetic retinopathy can lead to serious eye problems, such as:
• Bleeding inside the eye’s gel-like substance (vitreous), known as vitreous hemorrhage which can cause floating spots.
• Retinal detachment leads to visual field loss.
• Glaucoma, a condition when eye pressure is increased.
• Blindness, especially if the condition is not well-managed or is accompanied by macular edema or glaucoma.
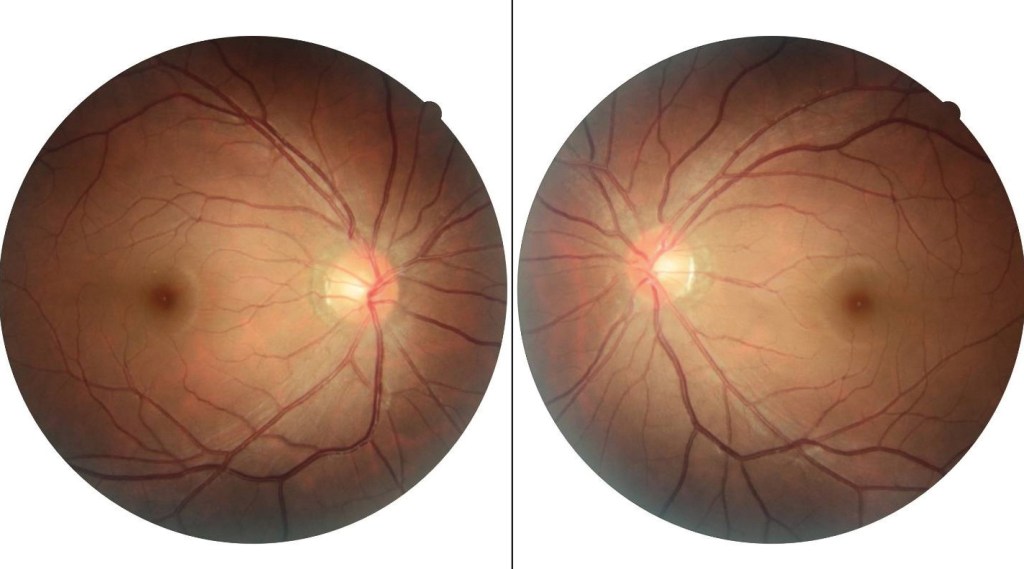

Images by Dr. Lim Chang Zhen
When to See an Eye Doctor:
For Type 1 Diabetes, initial eye screening should occur within 3-5 years of diabetes onset. Type 2 Diabetes individuals should undergo eye screening at the time of diabetes diagnosis. Pregnant women with pre-existing diabetes should have an eye examination before pregnancy, in the first trimester, and then close follow-up throughout pregnancy and the postpartum period.
Follow-up Eye Examination:
After the initial screening, individuals with diabetes should have annual eye examinations, even if there are no signs of diabetic retinopathy. More severe cases of diabetic retinopathy may require more frequent eye examinations. Regular and thorough eye exams are essential for preventing vision loss in individuals with diabetes. If you experience sudden changes in your vision, such as blurriness, spots in your visual field, floaters, or haziness, it’s crucial to promptly visit your eye doctor.
Treatment of Diabetic Retinopathy:
Treatment options include:
– Injections: Anti-VEGF drugs injected into the eye can slow down or reverse swelling in the retina.
– Laser Therapy: Used to shrink abnormal blood vessels, stop leakage, and reduce swelling in the retina.
– Eye surgery: In cases of excessive bleeding, scars, or retina detachment, vitreo-retina surgery may be required.

Image by Shroff Eye Centre
Prevention:
While diabetic retinopathy cannot be entirely prevented, several steps can reduce its risk, including:
– Controlling diabetes through a healthy lifestyle, including diet, exercise, and compliance with prescribed medications.
– Regularly monitoring blood sugar levels as advised by healthcare providers.
– Managing blood pressure and cholesterol through lifestyle changes or medications.
– Quitting smoking or using tobacco products, as smoking elevates the risk of diabetic complications.
– Remaining vigilant for any vision changes and promptly consulting an eye doctor.
Conclusion:
Optimal control of diabetes is crucial to avoid its complications, especially diabetic retinopathy. By closely monitoring blood sugar levels, following prescribed treatment regimes, living a healthy lifestyle, and undergoing regular eye check-ups, individuals can significantly lower their risk. Early detection and timely intervention are essential for effective treatment and preserving vision.

Dr. Lim Chang Zhen
Consultant Eye Physician
& Surgeon
MD (VSMU), M. Med. (Ophthalmology) (USM)
Dr. Lim Chang Zhen has developed expertise in various procedures and surgeries. His areas of specialisation encompass cataract surgery with premium lenses, diabetic retinopathy, eye infections, glaucoma, laser treatment, and pterygium surgery. Dr. Lim ensures that his patients receive the highest standard of care, incorporating the latest advancements in the field of ophthalmology.




