If you or your child ever had these skin problems, the answer may well be a yes! It is estimated that about 20% of children and 10% of adults suffer from a condition called ECZEMA.
What is eczema?
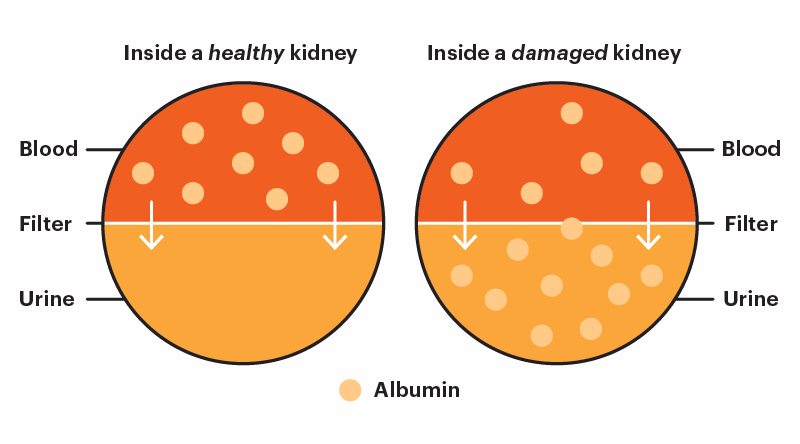
Eczema is the medical term for a skin condition that causes dry, itchy and inflamed rashes on the skin. It is a common condition in young children but it can occur in almost any age group. It is not contagious. The skin barrier helps your skin to retain moisture and protects your body from outside elements. When eczema happens, the skin barrier is weakened. This will allow bacteria, viruses, irritants and allergens to enter the body easily.
What are the Symptoms?
Initially, itchy rashes and skin dryness are first noticed. Depending on the patient’s skin colour, the rash can be red, pink or brownish in colour. Rubbing or scratching worsens the rash so it is often called “the itch that rashes.” The itch is usually worse in the evening triggered by sweating or rough clothing. It tends to involve the face, neck, elbow, elbow folds, knee and at the back of knees. Close family members with similar skin problems make the diagnosis more likely.
Who is prone to eczema?
Almost anyone of any race or gender can have eczema at any age. However, it tends to begin in the first 2 years of life but some may develop it even after puberty or during adulthood. Those with a family background of atopy (i.e eczema, bronchial asthma and allergic rhinitis) are more likely to get it.

What makes eczema worse?
• Climate: extremes of temperature, low humidity
• Irritants: wool/ rough fabrics, perspiration, detergents
• Infections: skin infections or other infections
• Environmental allergies: dust mites, pollen
• Food allergies: common allergens- eggs, milk, peanuts, shell fish, soy, wheat
(Note: detection of allergen specific Ig E via blood does not necessarily mean that allergy triggers the eczema)

The impact?
Eczema can have a significant impact on a person’s daily life. When scratching results in a wound with itchiness and inflammation, a child may not want to bathe as he will suffer an unpleasant stinging sensation. Sleep will be disturbed leaving the child irritable. In school, they may be stigmatized and other children may be hesitant to interact with the child with eczema. As they grow older, they may become self-conscious of the way their skin looks. Fortunately, early diagnosis and effective treatment can help patients and family members deal with this skin condition.
When to consult a dermatologist?
When sensitive skin care regimes and avoidance of irritants fail to completely clear up the itchy rash, it is time to consult a dermatologist. You or your child may need more potent treatment. Alternatively, it is possible that the rash is not due to eczema.
How do we treat eczema?
Upon diagnosing eczema, the dermatologist will prescribe topical products, such as topical steroids or calcineurin inhibitors as well as oral antihistamines. Other treatment options include phototherapy, wet wrap, systemic medications that target the immune system. Recently, newer oral and injectable monoclonal antibody have been proven effective.
Although eczema cannot be cured, it can be managed. Fortunately, some children’s symptoms lessen or disappear as they grow up. Hence, eczema should be diagnosed and managed early so that your child can thrive!
All photos credit: Dr. Janet Lee Hoong May

Dr. Janet Lee Hoong May
Consultant Dermatologist & Physician
MD (RSMU), MRCP (UK), Adv. Master in Dermatology (UKM)
Dr. Janet specialises in a variety of skin, scalp, hair and nail disorders for both adults and children i.e. acne, psoriasis, eczema, skin allergy and allergic testing, skin pigmentations, skin cancers, skin infections as well as hair loss. She has vast experience in dermatological procedures such as skin biopsy, electrocautery and excision, intralesional injections, cryotherapy, lasers and chemical peeling.