Understanding Metabolic Syndrome
Metabolic syndrome is a serious health condition that affects people from all walks of life, especially in countries where obesity and sedentary lifestyles are increasing at an alarming rate. It refers to a cluster of interconnected risk factors that, when present together, substantially increase the likelihood of developing chronic diseases such as type 2 diabetes, cardiovascular disease, stroke, and non-alcoholic fatty liver disease.
The five key risk factors that define metabolic syndrome are1:
- Abdominal obesity (waist circumference ≥90cm in Asian men or ≥80 cm in Asian women; waist measurement not needed if BMI >30 kg/m2)
- High triglycerides (≥1.7 mmol/L or currently taking medication for elevated triglycerides)
- Low HDL cholesterol (<1.03 mmol/L in men, <1.29 mmol/L in women or currently on treatment)
- Elevated blood pressure (≥130/85 mmHg or on antihypertensive treatment)
- Elevated fasting blood glucose (includes insulin resistance, impaired fasting glucose, impaired glucose tolerance, or on treatment)
A person is diagnosed with metabolic syndrome if they meet three or more of these criteria.
Why You Should Care
Metabolic syndrome significantly increases the risk of long-term health problems. What makes it especially dangerous is its silent progression. Many individuals have no symptoms and remain unaware of the dangers until they experience a major health event, such as a heart attack or stroke. You might feel fine and look fine, but your body could be struggling internally.
Targeting the Core: Why Abdominal Fat Deserves Attention
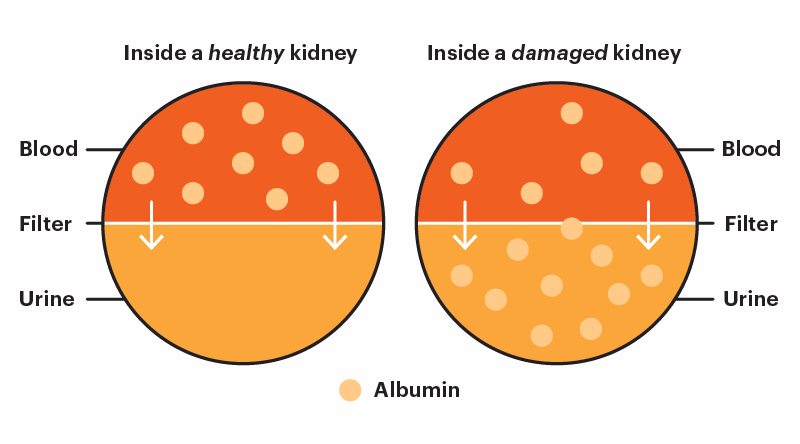
Central obesity plays a pivotal role in metabolic syndrome. Visceral fat — the fat stored deep inside the abdomen around vital organs — is metabolically active and harmful1. It releases cytokines and pro-inflammatory hormones that disrupt insulin regulation, blood pressure, and lipid metabolism1. As a result, a normal weight does not always mean a healthy body — people with hidden visceral fat can still face serious health risks.
Abdominal fat is more than a cosmetic issue — it’s a key contributor to metabolic problems, particularly insulin resistance. Insulin resistance impairs the ability of cells to absorb glucose, leading to high blood sugar levels and forcing the pancreas to produce more insulin to compensate1. Over time, this overwork can exhaust the pancreas’ beta cells, eventually leading to type 2 diabetes.
Are You Unknowingly at Risk?
Anyone can develop metabolic syndrome. While the risk increases with age, it’s no longer just a problem for older adults. Alarmingly, more cases are now being seen in young adults and even teenagers — largely due to poor lifestyle habits2.
You’re more likely to develop metabolic syndrome if you have:
- A family history of type 2 diabetes, high blood pressure, or heart disease
- A sedentary lifestyle (not enough physical activity)
- An unhealthy diet high in calories, sugar, saturated fat, or processed food
- Excess abdominal fat (visceral obesity)
Spotting the Red Flags
Early detection is crucial. Raising awareness about regular health check-ups is essential. These check-ups should include waist circumference, blood pressure, and fasting blood tests to measure glucose and cholesterol levels.
Many people with metabolic syndrome don’t show symptoms, which makes regular screening even more important. Everyone should be encouraged to monitor key health indicators: waist size, blood pressure, blood sugar, and cholesterol. Don’t wait for symptoms — prevention starts with action.
From Risk to Recovery: A Practical Approach
Metabolic syndrome can often be reversed in its early stages through sustained lifestyle changes, especially when it hasn’t yet led to severe complications.
Here are simple, non-medication-based steps to manage and possibly reverse metabolic syndrome:
- Maintain a Healthy Weight
Even a modest weight loss of 5–10% of your body weight can improve blood pressure, cholesterol, and insulin sensitivity. - Adopt a Balanced Diet
Eat more fruits, vegetables, whole grains, and lean proteins to support overall health; reduce sugary drinks, refined carbs, processed snacks, and fried foods to improve metabolic balance; and choose natural, unprocessed foods whenever possible to minimise hidden sugars and unhealthy fats. - Exercise Regularly
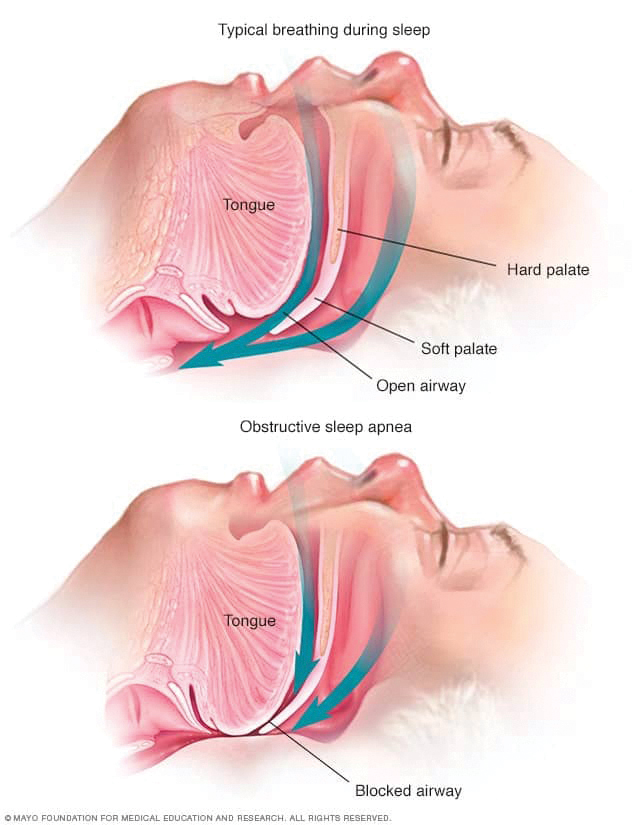
Aim for at least 150 minutes of exercise per week. Walking, cycling, swimming, and strength training are all helpful. Physical activity burns visceral fat and improves insulin function. - Sleep Well
Lack of quality sleep disrupts hormone balance, raises cortisol levels, and worsens insulin resistance — all of which are linked to weight gain. Individuals should aim for 7–9 hours of restful sleep each night. - Manage Stress
Chronic stress raises cortisol, which increases fat storage and disrupts blood sugar levels. Relaxation techniques like deep breathing and yoga can help restore balance.

In some cases, medication may be needed to better control blood pressure, blood sugar, or cholesterol. However, it’s important to remember that medication supports — but does not replace — lifestyle changes. A combined approach is key to reducing long-term health risks.
It’s also important to work closely with a healthcare provider to create a personalised health plan that suits your lifestyle and needs.
Final Thoughts
Metabolic syndrome may be common and serious, but it is also largely preventable — and often reversible with timely changes in your lifestyle. Raising awareness is just the start. Taking consistent action is what truly protects your health.
Make your health a priority — now and always.
1 International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome [internet]. Brussels: IDF; 2006 [cited 2025 Jun 27]. Available from: https://IDF.org/media/uploads/2023/05/attachments-30.pdf
2 Al-Hamad D, Raman V. Metabolic syndrome in children and adolescents. Transl Pediatr. 2017 Oct;6(4):397–407. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5682379/

Dr. Fang Li Chen
Consultant Physician
MD (UNIMAS), MRCP (UK)
Dr. Fang possesses a strong passion for internal medicines and demonstrates comprehensive expertise in a broad spectrum of medical and surgical pathologies. Her keen clinical acumen has consistently contributed to accurate diagnoses and effective patient management. Beyond clinical care, Dr. Fang is deeply committed to advancing patient well-being. She actively empowers individuals to take ownership of their health through evidence-based lifestyle interventions, stress management strategies and appropriate pharmacological treatments.