by Dr. Yeo Geok Ping,
Consultant Nephrologist & Physician
In National Health and Morbidity Survey 2019, the prevalence of Diabetes Mellitus (DM) amongst adults age >18 years old had increased from 11.2% (2011) to 18.3%.(2019). Over time, DM may lead to serious complications like heart attacks, strokes, kidney disease, vision loss, and nerve damage. DM remains the most common cause of End Stage Kidney Disease (ESKD), accounting for 53% of all new ESKD patients in 2021, followed by hypertension (33.9%).
How diabetes cause kidney disease?
Kidneys are two bean-shaped organs, each about the size of a fist located in the middle of your back, just below your ribcage. Each kidney is made up of millions of tiny filters called nephrons. These filters help to remove waste and excess water from the blood into the urine while leaving protein and other substances in blood. Kidneys also help to control blood pressure, produce red blood cells and activate Vitamin D. Over time, high blood sugar from diabetes can damage blood vessels in the kidneys as well as nephrons so they don’t work as well as they should. Around 20-30% of people with diabetes develop Diabetic Kidney Disease.
How to detect Diabetic Kidney Disease (DKD)?
Diabetic Kidney Disease (DKD) is kidney damage caused by DM. When the kidneys are working normally, they prevent albumin from leaking into the urine. Hence, the earliest sign of DKD is increased excretion of albumin in the urine. The kidney doctor (nephrologist) will perform assessment and screen for kidney damage by doing blood and urine tests.
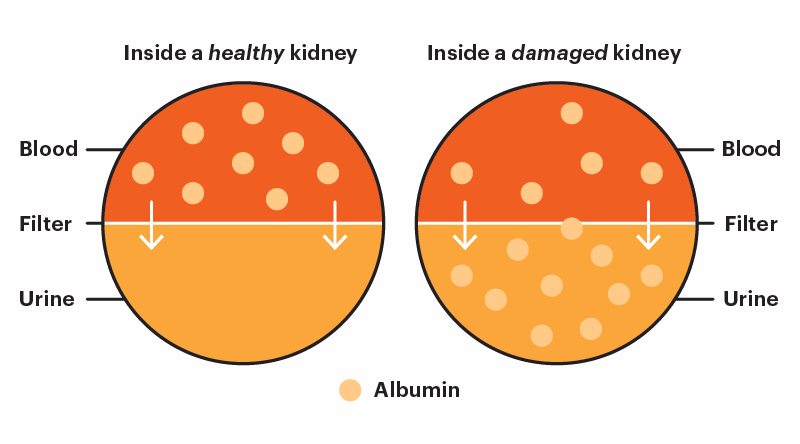
Photo credit: Diabetes and Digestive and Kidney Diseases (NIDDK)/kidney.org
Screening tests may include:
1. Urine test to measure excretion of albumin in urine.
2. Blood test to measure level of creatinine. It can estimate how well the kidneys filter blood. High creatinine indicates a low eGFR (estimated Glomerular Filtration Rate), indicating poor kidney function.
3. Ultrasonography of kidneys to assess the size of kidneys. The kidneys are usually normal or increased in size in the initial stages but later may shrink as the disease progresses.
What happens if there is kidney failure?
There are five stages of Chronic Kidney Disease (CKD). It is a silent killer as it may progress insidiously over time without any clinical manifestation. Eventually, DKD may cause the kidneys to shut down, leading to the last stage (stage 5) of CKD, known as End Stage Kidney Disease (ESKD).
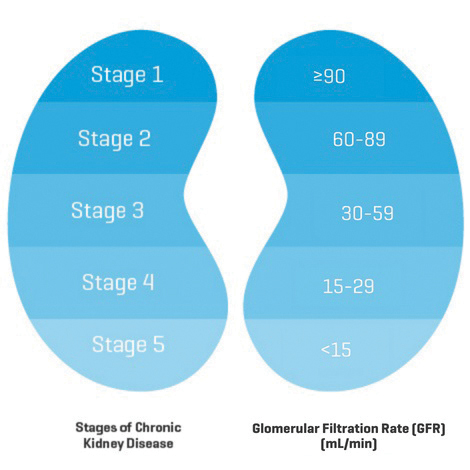
Photo credit: Baxter/mykidneyjourney.com
Symptoms and signs of kidney failure include:
• Nausea and vomiting
• Fatigue
• Swelling in the face, ankles and feet
• Breathlessness
• High blood pressure
• Confusion
• Dry skin and itchiness
• Anemia
ESKD occurs when the kidneys can barely function to meet day-to-day requirements. In this final stage, dialysis or kidney transplant is a must in order to survive. Kidney transplant involves the transfer of a healthy kidney from one person into the body of a person who has little or no kidney function. Kidney transplantation is the optimal treatment for improving survival and quality of life for patients with ESKD.
There are two types of dialysis treatments available to remove toxin and extra fluids from the body. Haemodialysis will require a machine that removes blood from the body, filters it through a dialyzer (artificial kidney) and returns the cleaned blood to body via vascular access either arteriovenous fistula (AVF) or dialysis catheter. Every Haemodialysis will be individualized but generally it takes an average of 4 hours per session and 3 treatments per week. Peritoneal Dialysis is dialysis using the peritoneal membrane, which is the natural lining of abdomen, via a tenckhoff catheter that is surgically placed in the abdomen. Continuous Ambulatory Peritoneal Dialysis (CAPD) is carried out manually every day. There are usually 4 exchanges during the day. Automated Peritoneal Dialysis (APD) requires a machine to perform three to five exchanges during the night while sleeping.
How do we treat Diabetic Kidney Disease (DKD)?
There is no medication or therapy that can reverse the kidney damage done. However, with the correct treatment, we can slow down the progression of DKD:
• Lifestyle modification : Stop smoking, regular exercise (At least 150 minutes per week)
• Healthy diet: Low salt and sugar.
• Good sugar control : The treatment will be individualized to prevent development of hypoglycaemia (low blood sugar)
• Good blood pressure control: Recommended goal below 130/80 mmHg, however target should be individualized.
• Avoid over-the-counter pain medication including non-steroidal anti-inflammatory drugs (NSAIDS) or non-FDA approved supplement.
• Compliance to medications and follow up are of paramount importance to retard the disease progression of DKD.
Time is critical in the treatment of kidney disease. The key point here is to have early diagnosis and treatment without delay, in order to minimize loss of kidney tissue from the injury.
Therefore, it is imperative to consult a nephrologist early, in order for a prompt diagnosis and initiation of treatment.
Sidenote:
Having foamy urine?
This could be your kidneys ‘leaking’ protein, the earliest sign of kidney disease.
“Time is kidney”
A key point here is to have early diagnosis and treatment as soon as possible without losing time, in order to minimize loss of kidney tissue from the injury.

