One of the most common complaints that doctors receive in their daily practice is severe menstrual pain. Most of the time, we may mistake the pain as normal menstrual pain and often endometriosis might be overlooked. Many studies have shown that the diagnosis of endometriosis can be delayed up to 10 to 12 years. The delay in diagnosis of endometriosis could severely affect the fertility of many women while some women develop complications such heavy menstrual bleeding, low blood levels (anaemia), having painful enlarged uterus (adenomyosis) or ovarian endometriotic cysts. At present, there is no objective test to diagnose this disease. Doctors depend on patient’s signs and symptoms to make a clinical diagnosis.
What is endometriosis?
Endometriosis is derived from the word “endometrium,” which is the tissue that lines the womb (uterus). Patients with endometriosis have endometrial type of tissue which grows outside of the uterus particularly in the surrounding organs such as bladder, bowels and sometimes, even in the distant parts of the body such as the umbilicus, lungs and the brain.
The endometriotic lesion is influenced by the female hormones. It undergoes proliferation, break downs and bleeds during each menstrual cycle. Its characteristics resemble a normal endometrial tissue which is found inside the womb. With each menses, endometriosis will cause chronic inflammation and the formation of scar tissues inside the pelvis, which can distort the anatomy of the surrounding organs and interfere with their functions.
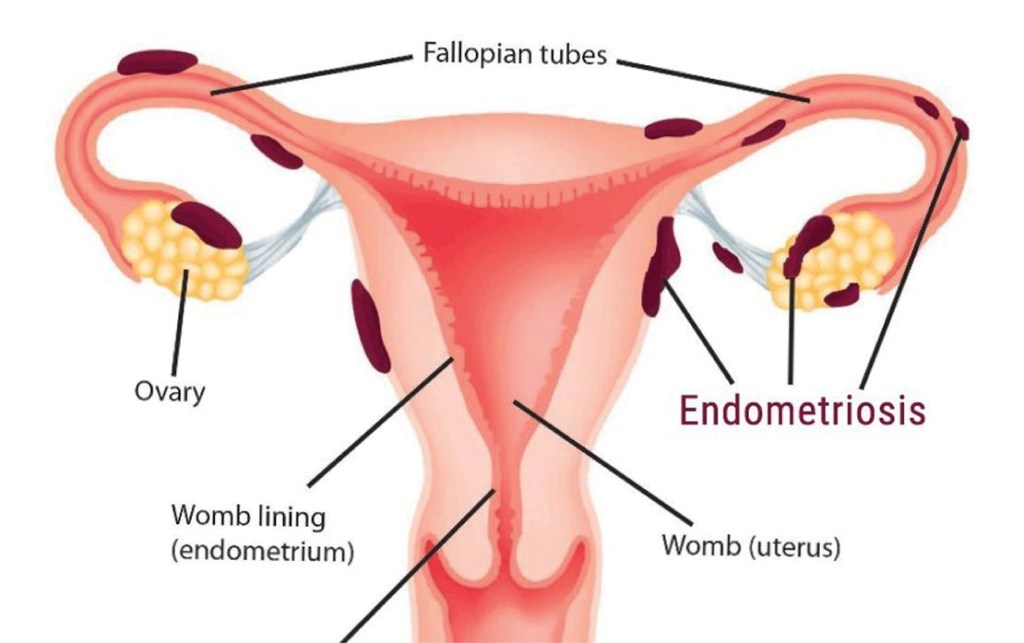
Endometriosis tissues implant outside the uterus
What causes endometriosis?
Doctors and researchers have not identified the cause of endometriosis. One of the most popular and widely believed theory is Sampson’s Theory of Retrograde Menstruation, postulated by Dr. John Sampson in the 1920’s. According to the theory, during each menstrual cycle, a certain amount of menstrual fluid in the uterus is forced into the pelvic cavity via the fallopian tubes. The body usually responds to this kind of spilling by reabsorbing the menstrual fluid back into the circulatory system. However, in some women, due to immune system dysfunction, the fluid is not reabsorbed but instead implants itself and grows on the pelvic and abdominal organs.
We also realise that endometriosis tends to run in families. If your mother or sister has endometriosis, you’re more likely to get it. Research shows that it tends to get worse from one generation to the next.
What are the symptoms and signs of endometriosis?
1. Pelvic pain
Most women with endometriosis experience severe pelvic pain, lower back pain and cramps before and during menstruation. The medical term for such severe pain is called dysmenorrhea. Other common complaints include dyspareunia (pain during intercourse), dyschezia (painful defecation) and dysuria (painful urination).
2. Heavy or irregular vaginal bleeding
Women with endometriosis may experience excessive menstrual bleeding or bleeding between periods.
3. Infertility
Some women with endometriosis may experience little or no pain at all but are unable to conceive and are usually first diagnosed with endometriosis while seeking treatment for infertility. These are usually cases where the formation of scar tissue (adhesions) due to endometriosis, has somehow distorted the reproductive organs and therefore results in inability to conceive.
4. Painful bowel movements
Some women may experience bowel pain followed by abdominal bloating, constipation, or diarrhoea. The pain may intensify during menstruation.
Diagnosis
There are no specific tests to assess whether a woman has endometriosis. Exploring a patient’s medical history may give the doctor some clue to the presence of this disease, and it is usually accompanied by a pelvic examination.
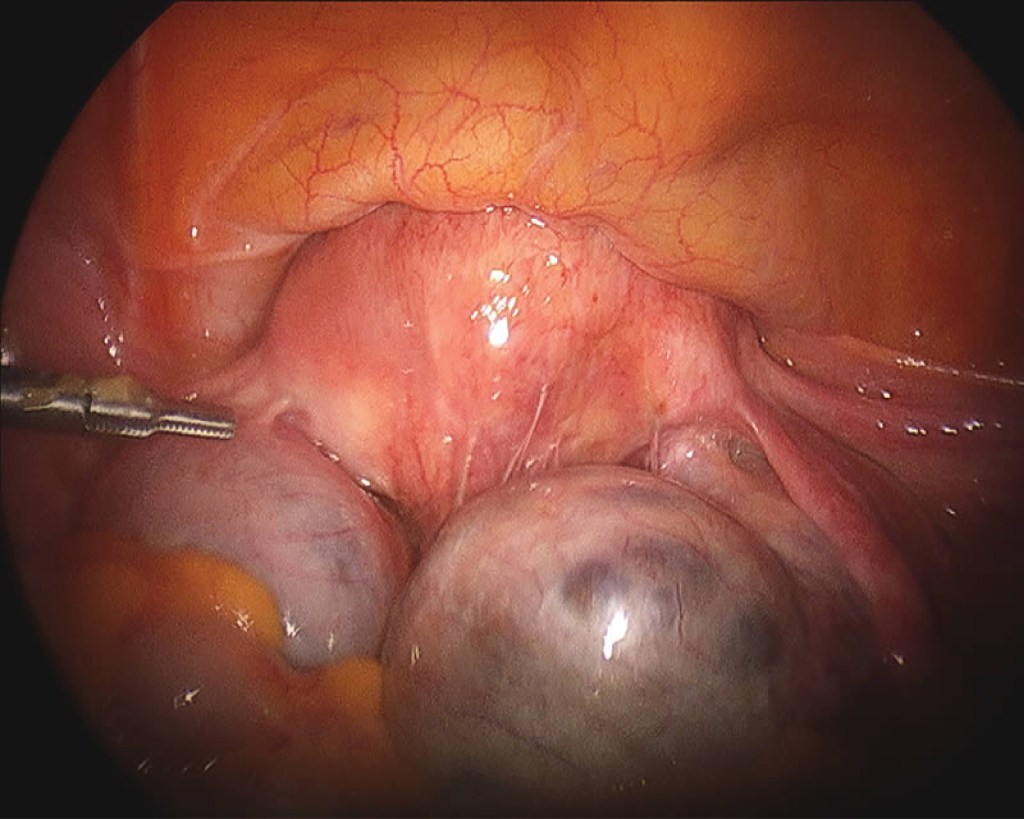
The pelvic examination may reveal irregular painful swellings in the Pouch of Douglas and an enlarged uterus. The pelvic ultrasound may reveal ovarian cysts that appear in the form “kissing cysts” (picture below). Sometimes, the doctor may order a blood test called CA-125 and if it is elevated, it is suggestive of endometriosis.
In some cases, it is possible to be mistaken endometriosis for other gynaecological conditions that have similar symptoms and vice versa. The only reliable way to confirm and verify the suspected diagnosis of endometriosis is through laparoscopy.

Transvaginal ultrasound shows bilateral endometriotic cysts

Endometriotic tissues can implant in between uterine muscle walls causing enlarged uterus, heavy menses and severe menstrual pain. The enlarged uterine wall is known as adenomyosis.
Treatment Options
There is no cure for endometriosis now and this condition can be difficult to treat. The aim of treatment is to relieve pain, to remove endometriotic tissues to improve fertility and to prevent disease recurrence. Treatment modalities can be divided into 3 categories:
a) Pain killers
b) Surgery
c) Hormonal therapy
a) Pain killers
Non-steroidal anti-inflammatory drugs (NSAIDs) are medicines that are widely used to relieve pain, help to reduce inflammation, and bring down a fever; for example, ibuprofen and mefenamic acid. They can be used together in combination with paracetamol for more severe pain. These painkillers are available in pharmacies.
b) Surgery
Surgery is the main treatment option for women with endometriosis. Laparoscopic surgery (key hole) is the preferred surgery but sometimes we may need to perform open laparotomy for very complicated cases. The aim of surgery is to diagnose endometriosis as well as to remove as much of the diseased areas as possible.
c) Hormonal therapy
Endometriosis is influenced by the hormone oestrogen. Whenever there is menstruation, the endometriotic lesion will grow, causing pain and forming adhesions in the pelvis. By giving hormonal therapy, menstruation is reduced or suppressed and therefore prevents the growth of endometriosis and relieve its symptoms. Hormonal therapies can be given before and essentially after laparoscopic surgery to suppress any remaining tissues. Some of the therapies include:
i. Gonadotropin-releasing hormone (GnRH) agonist
ii. Combined oral contraceptive pills
iii. Progestogens pills
iv. Mirena® (intrauterine device coated with hormone)

Can endometriosis recur after surgery?
Endometriosis can recur after surgery and medical treatment. The chance of recurrence is higher if endometriotic lesions are not excised completely. If the patient is not contemplating pregnancy immediately after the surgery, continuing medical therapy after surgery to suppress any endometriotic lesion that has not been excised.
Complimentary Therapies
Although there is only limited evidence for their effectiveness, some women may find the following therapies helpful to reduce pain and improve their quality of life:
• reflexology
• transcutaneous electrical nerve stimulation (TENS)
• acupuncture
• vitamin B1 and magnesium supplements
• traditional Chinese medicine
• herbal treatments
• homeopathy
Is endometriosis associated with ovarian cancer?
Studies have shown that patients with ovarian endometriosis have 2-3-fold increased risk of ovarian cancer.
Should pregnancy be recommended as a treatment for endometriosis?
Pregnancy might help to reduce endometriosis symptoms only temporarily, but it is not a cure. There are also risks involved, as women with endometriosis are more likely to have pre-term births, increased rates of caesarean sections and an increased risk of miscarriages.
Are there ways to prevent endometriosis?
Endometriosis is an idiopathic condition, meaning there is no known cause. There are also no specific ways to prevent endometriosis. However, being aware of the symptoms and whether you could be at higher risk can help you know when to discuss it with a doctor.
Summary
Women with endometriosis constantly battle with monthly pelvic pain, and it affects their fertility. Being pregnant with endometriosis may also increase your risk of serious pregnancy complications. Therefore, women should seek consultation with their gynaecologists for an early diagnosis. With early intervention, it may improve their quality of life and reduce severe complications.
Dr. Chua Shih Keat
Obstetrician & Gynaecologist
MD(UPM), MRCOG(UK)
Dr. Chua Shih Keat received his medical degree from Universiti Putra Malaysia and obtained the membership of Royal College of Obstetricians and Gynaecologists (MRCOG), United Kingdom.
Dr. Chua specializes in the care of women during pregnancy and childbirth and in the diagnosis and treatment of diseases of the female reproductive organs. He has been managing women’s health issues for the past 16 years in various health facilities.


