What is lymphoma?
Lymphoma is a cancer of the lymphatic system, which is part of the body’s immune system. The lymphatic system consists of lymph nodes, tonsils, spleen, thymus gland and bone marrow. Lymph fluid contains white blood cells which defend the body against invasion by bacteria, viruses, parasites and other foreign substances. Lymphoma develops when white blood cells called lymphocytes grow out of control.
What are types of lymphoma?
There are two major types of lymphomas: Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL), which differ in the way they develop and spread, as well as in the way they are treated. The World Health Organization (WHO) divides HL into two main groups: classical HL (cHL) and nodular lymphocyte-predominant HL (NLPHL). Most patients with HL are diagnosed between 15 and 30 years of age, followed by another peak in adults aged 55 years or older. For NHL, it is a heterogenous group of blood disorder arises from B-lymphocytes, T-lymphocytes, or natural killer (NK) cells. There are more than eighty subtypes of NHL, which can be simplified into two major categories, namely B-cell and T/NK-cell NHL.
What is the incidence of lymphoma?
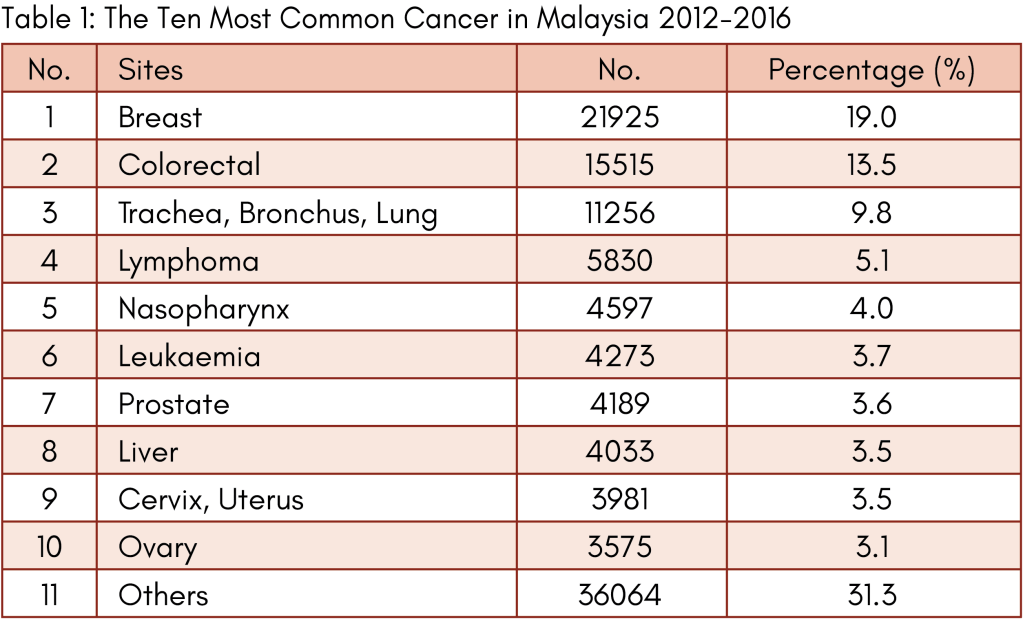
NHL is more common than HL. Most NHL (85-90%) are from B cells and less than 15% develop from T cells. Classical and nodular lymphocyte predominant HL account for 95% and 5% of all HL respectively. According to Malaysia National Cancer Registry Report 2012-2016, lymphoma is the fourth most common form of cancer overall in Malaysia after breast, colorectal and lung malignancies (table 1).
What causes lymphoma?
The causes of lymphoma are not understood. However, people with certain risk factors have a slightly higher chance of developing lymphoma compared with people without these risk factors. Known risk factors for lymphoma include:
1. Immunodeficiency: HIV infection, transplantation, Wiskott-Aldrich syndrome.
2. Infection: human T-cell lymphotropic virus type 1, Epstein-Barr virus, helicobacter pylori.
3. Autoimmune: Crohn’s disease, systemic lupus erythematosus, Sjogren syndrome.
4. Environmental toxins: pesticides, herbicides, certain drugs used to treat cancer.
While siblings and children of patients with lymphoma have a slightly increased risk of developing this disease compared with the general population, there are no clearly identifiable genetic or hereditary factors that can predict this slightly increased risk. Therefore, routine screening for lymphoma among the immediate family members of patients with lymphoma is not recommended.
What are the symptoms?
Some patients with lymphoma do not have any obvious signs or symptoms of the disease. The clinical features at presentation reflect a spectrum from low grade to high grade lymphoma. Low grade (also called indolent) lymphomas usually grow slowly, exhibit few symptoms, typically present with widespread disseminated disease at diagnosis and are generally not curable. Patients can live a long time with indolent lymphomas because they tend to respond well to treatment and can remain in remission for many years or even decades. However, over time, some indolent lymphomas may transform into high grade lymphomas.
High grade lymphomas (aggressive lymphomas) grow and spread more quickly than low grade lymphomas. Destructive growth pattern of the deep lymph nodes within the chest or abdomen may press against various internal organs, causing difficult breathing, cough, poor appetite, weight loss, abdominal pain and distension, constipation, fever and legs swelling. Many patients with aggressive lymphomas can be cured by chemotherapy that kill rapidly dividing tumour cells.
Anyone who has an enlarged lymph node that does not return to normal size within few weeks and/or persistent symptoms should see a doctor immediately to make sure that lymphoma or another serious condition is not present.
How is the diagnosis made?
An accurate pathologic diagnosis is the most important first step in the management of lymphomas. An incisional or excisional lymph node biopsy in combination with immunohistochemistry (IHC) is recommended to establish the diagnosis of lymphoma. IHC is essential for the differentiation of various subtypes. Fine needle aspiration (FNA) is inadequate for reliable diagnosis and grading. Other special test includes cytogenetic analysis, which involves examination of chromosomes from lymphoma cells under a microscope to check for any abnormalities in number or structure. The result of cytogenetic analysis often helps doctors to determine which type of lymphoma a patient has.
What is the workup for lymphoma?
Essential workup procedures include:
1. Physical examination
2. Laboratory: blood count, lactate dehydrogenase, metabolic panels, hepatitis viruses, HIV
3. Bone marrow aspiration, trephine biopsy +/- immunophenotyping (for staging purpose).
4. Imaging: chest X-ray, CT neck, chest, abdomen, pelvis (for staging purpose)
5. Electrocardiograph (ECG) and echocardiogram
6. Optional: PET CT scan, lumbar puncture, brain MRI (depending on subtype & site)
What are the treatment options available?
Treatment results for lymphomas have improved dramatically over the past four decades. The advent of more effective treatment options has improved the 5-year survival rates. Treatment for lymphoma varies widely based on the subtype. Treatment options include:
1. Watchful waiting (for low grade lymphomas)
2. Chemotherapy +/- immunotherapy (monoclonal antibody)
3. Radiotherapy
4. Stem cell transplantation (autologous, allogeneic)
5. Chimeric antigen receptor (CAR) T-cell therapy
6. Novel agents
7. Clinical trials
What is the prognosis?
The prognosis is based on the stage at which the disease is diagnosed and determined by the lymphoma subtype, in addition to other factors such as performance status, age and other medical issues. Treatment for HL is highly effective and most patients are eventually cured. The survival rate for HL is generally higher than that of NHL. The American Cancer Society reports 5-year overall survival rate of 80% for HL and 72% for NHL. Various prognostic indices have been developed for different forms of lymphoma. The International Prognostic Index (IPI) was developed for aggressive NHL and validated in all clinical grades of NHL as a predictor of response to therapy, relapse and survival. The IPI is based on five factors: age, performance status, lactate dehydrogenase level, number of extra-nodal sites and stage of the disease.

Dr Teoh Ching Soon
Clinical Haematologist &
Physician
MD (UPM), MRCP (UK), F’ship in Clinical Haematology (Malaysia), F’ship in Bone Marrow & Stem Cell Transplantation (Taiwan)
Dr Teoh Ching Soon is the Clinical Haematologist & Physician in Loh Guan Lye Specialists Centre. He has a keen interest in the management of malignant haematological disorders such as leukaemia, lymphoma, multiple myeloma, myelodysplastic syndrome and myeloproliferative neoplasm. His clinical work also focuses on benign haematological diseases, red cell and platelet disorders, coagulation and haemostasis, consultative haematology and haematopoeitic stem cell transplantation.


